If you suffer from the throbbing, intense pain set off by migraine headaches, you may well wonder which medicines are most likely to offer relief. A recent study suggests a class of drugs called triptans are the most helpful option, with one particular drug rising to the top.
The study drew on real-world data gleaned from more than three million entries on My Migraine Buddy, a free smartphone app. The app lets users track their migraine attacks and rate the helpfulness of any medications they take.
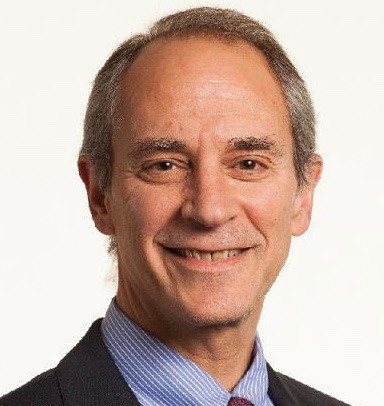
Dr. Elizabeth Loder, professor of neurology at Harvard Medical School and chief of the Division of Headache at Brigham and Women’s Hospital, helped break down what the researchers looked at and learned that could benefit anyone with migraines.
What did the migraine study look at?
Published in the journal Neurology, the study included self-reported data from about 278,000 people (mostly women) over a six-year period that ended in July 2020. Using the app, participants rated migraine treatments they used as “helpful,” “somewhat helpful,” or “unhelpful.”
The researchers looked at 25 medications from seven drug classes to see which were most helpful for easing migraines. After triptans, the next most helpful drug classes were ergots such as dihydroergotamine (Migranal, Trudhesa) and anti-emetics such as promethazine (Phenergan). The latter help ease nausea, another common migraine symptom.
“I’m always happy to see studies conducted in a real-world setting, and this one is very clever,” says Dr. Loder. The results validate current guideline recommendations for treating migraines, which rank triptans as a first-line choice. “If you had asked me to sit down and make a list of the most helpful migraine medications, it would be very similar to what this study found,” she says.
What else did the study show about migraine pain relievers?
Ibuprofen, an over-the-counter pain reliever sold as Advil and Motrin, was the most frequently used medication in the study. But participants rated it “helpful” only 42% of the time. Only acetaminophen (Tylenol) was less helpful, helping just 37% of the time. A common combination medication containing aspirin, acetaminophen, and caffeine (sold under the brand name Excedrin) worked only slightly better than ibuprofen, or about half the time.
When researchers compared helpfulness of other drugs to ibuprofen, they found:
- Triptans scored five to six times more helpful than ibuprofen. The highest ranked drug, eletriptan, helped 78% of the time. Other triptans, including zolmitriptan (Zomig) and sumatriptan (Imitrex), were helpful 74% and 72% of the time, respectively. In practice, notes Dr. Loder, eletriptan seems to be just a tad better than the other triptans.
- Ergots were rated as three times more helpful than ibuprofen.
- Anti-emetics were 2.5 times as helpful as ibuprofen.
Do people take more than one medicine to ease migraine symptoms?
In this study, two-thirds of migraine attacks were treated with just one drug. About a quarter of the study participants used two drugs, and a smaller number used three or more drugs.
However, researchers weren’t able to tease out the sequence of when people took the drugs. And with anti-nausea drugs, it’s not clear if people were rating their helpfulness on nausea rather than headache, Dr. Loder points out. But it’s a good reminder that for many people who have migraines, nausea and vomiting are a big problem. When that’s the case, different drug formulations can help.
Are pills the only option for migraine relief?
No. For the headache, people can use a nasal spray or injectable version of a triptan rather than pills. Pre-filled syringes, which are injected into the thigh, stomach, or upper arm, are underused among people who have very rapid-onset migraines, says Dr. Loder. “For these people, injectable triptans are a game changer because pills don’t work as fast and might not stay down,” she says.
For nausea, the anti-emetic ondansetron (Zofran) is very effective, but one of the side effects is headache. You’re better off using promethazine or prochlorperazine (Compazine), both of which treat nausea but also help ease headache pain, says Dr. Loder.
Additionally, many anti-nausea drugs are available as rectal suppositories. This is especially helpful for people who have “crash” migraines, which often cause people to wake up vomiting with a migraine, she adds.
What are the limitations of this migraine study?
The data didn’t include information about the timing, sequence, formulation, or dosage of the medications. It also omitted two classes of newer migraine medications — known as gepants and ditans — because there was only limited data on them at the time of the study. These options include
- atogepant (Qulipta) and rimegepant (Nurtec)
- lasmiditan (Reyvow).
“But based on my clinical experience, I don’t think that any of these drugs would do a lot better than the triptans,” says Dr. Loder.
Another shortcoming is the study population: a selected group of people who are able and motivated to use a migraine smartphone app. That suggests their headaches are probably worse than the average person, but that’s exactly the population for whom this information is needed, says Dr. Loder.
“Migraines are most common in young, healthy people who are trying to work and raise children,” she says. It’s good to know that people using this app rate triptans highly, because from a medical point of view, these drugs are well tolerated and have few side effects, she adds.
Are there other helpful takeaways?
Yes. In the study, nearly half the participants said their pain wasn’t adequately treated. A third reported using more than one medicine to manage their migraines.
If you experience these problems, consult a health care provider who can help you find a more effective therapy. “If you’re using over-the-counter drugs, consider trying a prescription triptan,” Dr. Loder says. If nausea and vomiting are a problem for you, be sure to have an anti-nausea drug on hand.
She also recommends using the Migraine Buddy app or the Canadian Migraine Tracker app (both are free), which many of her patients find helpful for tracking their headaches and triggers.
About the Author

Julie Corliss, Executive Editor, Harvard Heart Letter
Julie Corliss is the executive editor of the Harvard Heart Letter. Before working at Harvard, she was a medical writer and editor at HealthNews, a consumer newsletter affiliated with The New England Journal of Medicine. She … See Full Bio View all posts by Julie Corliss
About the Reviewer
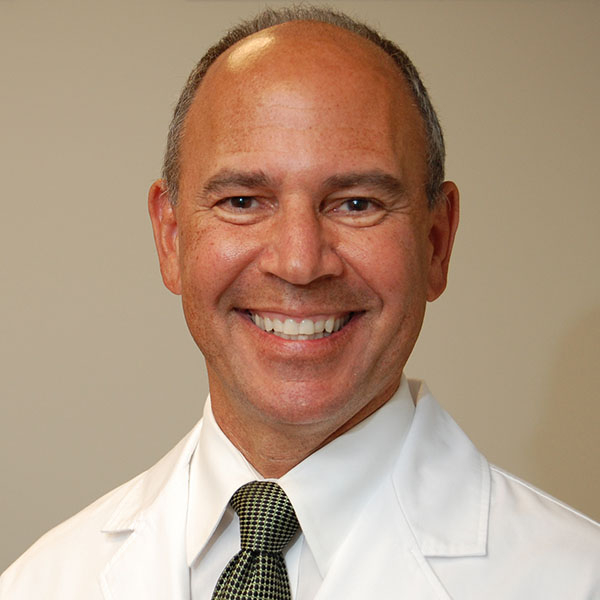
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD